Magnetic resonance imaging study of the in vivo position of the extraglottic airway devices i-gel™ and LMA-Supreme™ in anaesthetized human volunteers
Authors
Russo S.G. et al.
Publication
Br J Anaesth 2012; 109 (6): 996-1004.
Summary
- A study to compare the in situ position of the LMA Supreme™ and the i-gel™ supraglottic airway devices in anaesthetised volunteers
- The LMA Supreme™ protruded deeper into the upper oesophageal sphincter than the i-gel™, relative to both the glottis and to the spine
Objectives:
- To compare the in situ position of the LMA Supreme™ and the i-gel™ supraglottic airway devices in anaesthetised volunteers
Method:
- This prospective, randomised, crossover study was undertaken in human volunteers aged >18 years with a body weight of 60-80 kg and normal airways
- Subjects were American Society of Anesthesiologists physical status 1
- During the course of the study, both the LMA Supreme™ and the i-gel™ devices were evaluated in each volunteer in a randomised sequence
- The position of each device was visualised and compared using magnetic resonance imaging (MRI) of the head and neck, as well as fibre-optic and functional assessments
- The primary endpoint was the depth that the devices protruded into the upper oesophageal sphincter
- Other endpoints were
- The effect of the devices on airway calibre
- Distortion of other anatomical structures
Results:
- Overall, 6 male and 6 female volunteers were included in the study
- Subjects had a mean age of 25.8 years and a mean body mass index of 22.5 kg/m2
- Fibre-optic and functional assessments showed that the LMA Supreme™ and i-gel™ devices occupied anatomically identical positions, evidenced by
- Visible vocal cords and arytenoids (with no airway obstruction) in all subjects
- Device tips located distal to the arytenoids, extending into the hypopharynx
- Comparable leak pressures (LMA Supreme™, 20 cm H2O; i-gel™, 18 cm H2O)
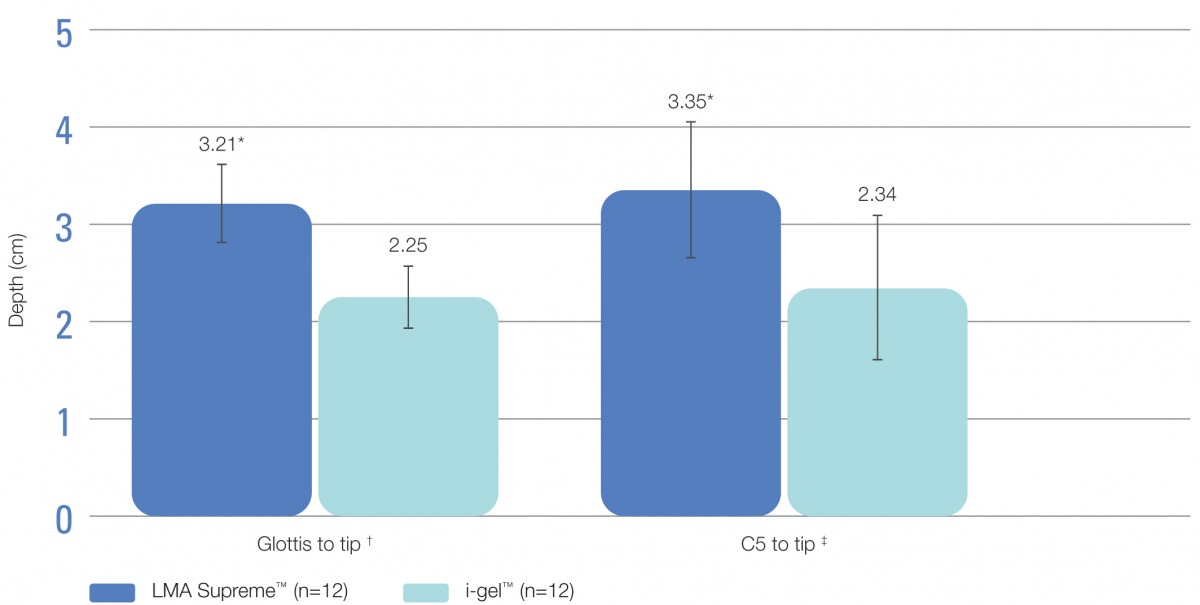
- The tip of the LMA Supreme™ protruded significantly (p<0.001) deeper into the upper oesophageal sphincter than the tip of the i-gel™, relative to both the glottis and to the spine (Figure 1)
- Dilation at the upper level of the upper oesophageal sphincter was significantly less with the LMA Supreme™ than with the i-gel™ (5.13 vs. 5.81 cm2; p=0.009)
- Dilation at the mid-level of the upper oesophageal sphincter was comparable with the two devices (3.69 vs. 3.79 cm2, respectively; p=0.65)
- Although both devices had a marked effect on laryngeal structures, compression of the laryngeal inlet was significantly (p=0.005) more pronounced with the LMA Supreme™ versus the i-gel™ (from 0.98 cm [native] to 0.51 cm and 0.62 cm, respectively)
- A significant (p<0.001) deflection of the epiglottis was observed with both devices (from 180° at baseline to 120° after insertion)
- The degree of deflection with both devices was comparable despite that the epiglottis was folded into the mask bowl in 1 subject fitted with the LMA Supreme™ and in 11 subjects fitted with the i-gel™
Figure 1. Depth of protrusion of the tip of the LMA Supreme™ and i-gel™ into the upper oesophageal sphincter (data are shown as mean ± standard deviation)
* p<0.001 vs. i-gel™ † Distance between the glottis and the distal tip of the device; ‡ Distance between the lower plate of vertebra C5 and the distal tip of the device
Conclusions:
- Fibre-optic and functional assessments showed that the LMA Supreme™ and i-gel™ devices occupied similar positions in situ in anaesthetised volunteers
- MRI showed that the LMA Supreme™ protruded deeper into the upper oesophageal sphincter than the i-gel™, relative to both the glottis and to the spine
- There were significant differences in the effects of the LMA Supreme™ and i-gel™ on adjacent soft tissues and airway calibre